Information about childbirth and the postpartum period - English
Information about childbirth and the postpartum period - English
Innhold
Informasjon på norsk og arabisk
Mental preparation
What are your expectations when it comes to childbirth?
Early on in your pregnancy, go over your thoughts on childbirth. Talk to each other, the midwife and others. Try to look forward to it!
Remember that childbirth is a positive, but exhausting, experience.
- You can practice breathing and relaxing. Find a method that works for you!
- Music and/or visualization. Think about how you have previously prepared yourself for physical or mental challenges (competitions, training, mountain treks, exams, etc.)
Childbirth
If your labour begins with contractions, you can often wait at home until they are regular and happen at five-minute intervals. If the water breaks or bleeding occurs, or if you experience strong abdominal pain or there is little foetal movement, contact the maternity ward at St. Olav’s University Hospital.
How does childbirth begin?
Blood show
Mucus plug: The mucus plug prevents infection in the uterus during pregnancy and can come out in the form of a mucous discharge or clump of mucus toward the end of the pregnancy. It indicates nothing with regard to when labour begins.
Blood show (bloody discharge/mucus) can be seen when the cervix dilates and child labour approaches.
Uterine contractions
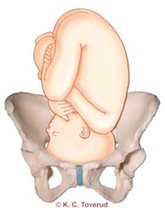
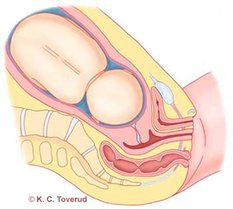
Each contraction begins in the top part of the uterus and spreads downward throughout the entire muscle through impulses. The child is shoved downward into the birthing channel. At the same time, the contractions cause the lower part of the uterus to open. The contractions come and go at regular intervals. It is important to work with the contractions (and not against them) and to keep your jaw open, your forehead relaxed, your hands open and your pelvic floor relaxed. Contact the maternity ward when the contractions last approximately 60 seconds and happen both regularly and approximately every 5 minutes.
Rupture of the amniotic membranes (water breaking)
The amount discharged varies from between 0.3-3 litres and its appearance is opalescent/shiny. The water can break before the contractions begin, during labour or when the child is born.
If the breaking is long-lasting (48 hours), labour will be induced. If the water has broken, you should contact the maternity ward whether you have contractions or not.
When should I contact the maternity ward?
- If the water breaks
- If you experience strong contractions
- If the child is very still and does not move
- If there is bleeding
- If you experience other abdominal pain than pain from contractions
More information on when you should go to the maternity ward is provided in this video:
Latent phase
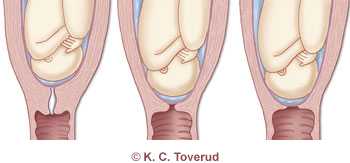
The latent phase is defined as the period lasting from when uterine contractions begin and until external cervical effacement occurs and there is an opening of 3-4cm.
The amount of time that this phase takes varies from woman to woman. For some women, it can last a long time (20 hours). It is important that you get enough rest and nutrition during this phase, because it is not certain that you will have much of an appetite later on in the birthing process.
Most women manage this phase well and wish to remain at home during it. The contractions are often short and not especially painful.
Arrival
The maternity ward asks that you call before arriving, so that it can be prepared to receive you. Call the maternity ward expedition at (+47) 72 57 57 77 and a midwife will speak with you.
Pointers on what you can take with you to the hospital
If you wish to communicate your thoughts with regard to the upcoming childbirth, you can write these down as a ‘wish list’. You can send the list to the maternity ward beforehand, so that it can be incorporated into the journal before you arrive, or take it with you when you come to be admitted.
When you arrive, go to the maternity ward expedition and a secretary will receive you there. Thereafter, a midwife will come and take you to one of the maternity wards (the ‘east ward’ or the ‘west ward’, depending on where you live or where there are the most spaces available when you arrive).
The midwife will ask how you are feeling and listen to the pulse of the child in your womb. Furthermore, she will measure your blood pressure, feel your belly to assess how the child is positioned and what your contractions are like. The midwife will assess how far along you have come in the birthing process through undertaking a vaginal examination, whereby she can feel how great the cervical opening is and how far down into the pelvis the child has come. As a rule, a vaginal examination is not undertaken if the water has broken without uterine contractions taking place.
If the midwife assesses that you are in the active phase of labour, you will remain at the maternity ward. If she assesses that you are still in the latent phase of labour and doing well, she may recommend that you take a walk home or around in the vicinity of the hospital to see if the contractions increases.
If you have not defecated during the lasts days before childbirth, it can be a good idea to give yourself a little enema when you enter the maternity ward. The problem will often take care of itself through much activity in your stomach/intestinal system when the contractions begins.
Active phase
The transition from the one phase of labour to the next is a smooth one. The active phase is considered to have begun when the cervix is dilated 3-4cm and uterine contractions occur more or less regularly.
The contractions occur at shorter intervals, last longer and are more intense and painful. This is a sign that they are now more effective.
Progress in the work of childbirth is now more rapid. The child is moving further down into the birthing canal and the cervix is dilating more rapidly than during the latent phase.
The midwife intermittently assesses how the child in the womb is doing as the birthing process progresses through listening to its pulse. To do so, she may use a wooden stethoscope, a hand-held Doppler-device or a CTG-device/STAN. The choice of method used is based on hospital and national guidelines.
You can read more about methods of foetal monitoring on St. Olav’s University Hospital’s webpages.
She assesses how things are going for you as an expectant mother and provides you with advice and guidance on how you can best manage the contractions and pain.
Progress in the birthing process
The midwife follows you up with regard to your progress in the birthing process through assessing the uterine contractions (how often they occur, for how long they last and how powerful they seem) and undertaking vaginal examinations (approximately every four hours, but more often if needed) to feel the cervical opening and how far down into the pelvis the child has come.

When you are in the active phase of labour, the birthing process is expected move forward. It may happen in fits and starts , but the cervix is expected to dilate approximately 1cm every 1-2 hours on the average. Often, the last centimetres of cervical dilation occur more rapidly than the first.
Sitting upright and being in motion during the cervical dilation phase is advantageous with respect to both progress in the birthing process and pain relief. Try to find a position where you feel that you can manage the contractions well. For example, you can stand upright and lean on a companion/wall bars/pulpit/bed, stand and rock your pelvis back and forth a little, walk around the room a little or stand on all four over the bean bag in the bed.
Food/drink
Childbirth is exhausting and you will need to eat/drink as you proceed, so that your body will be up to carrying out the work required. It can be a good idea to eat well during the starting phase of labour. When you are in the active phase, it is not certain that you will want to eat much. It is normal to lose one’s appetite and some women become nauseous and throw up.
It can be a good idea to bring with you light foods that provides energy (like energy bars, bananas, yoghurt, etc.) and to try to eat them as you proceed. It is also important that you drink regularly (sports drinks, for example, which are available at the maternity ward).
Also, being in a bathtub can be advantageous with respect to both pain relief and progress in the birthing process, as the body moves more freely and lightly in water and water can help you to relax your muscles.
If progress does not occur as expected, the midwife will stimulate uterine contractions to help the birthing process along.
If the cervix does not dilate or the child does not move down through the pelvis, a caesarean section must be performed (see procedures).
Transitional phase
The period right before full cervical dilation is called the transitional phase. The phase is often characterized by one feeling restless, irritable and discouraged. You may feel that you need more pain relief and that you cannot endure anymore. The contractions are at their strongest and most painful. Some may also experience a short pause in the contractions during this phase, a little break that is more than welcome.
You will need much support and encouragement from the midwife and your companion during this phase. Don’t give up. As a rule, it is almost over.
As the child’s head moves further down into the birthing canal and the cervix fully dilates, you will as rule experience a reflexive need to push, one that is difficult to oppose. You have reached the expulsion phase.
Some experience a need to push before the cervix is fully dilated. This may have to do with the child’s position in the pelvis. On the other hand, it may sometimes be caused by stools in the intestinal tract. Also, in cases where the water has not broken, a full bladder may trigger the need to push.
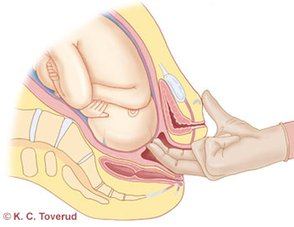
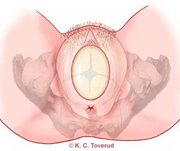
For women giving birth for the first time (nulliparous), it will in some cases be useless to push if the cervix is still a few centimetres short of full dilation, as pushing can then cause the cervix to swell and delay the process. The midwife will, therefore, undertake a vaginal examination when you feel the need to push, so that she can assess whether or not the time has come to begin pushing.
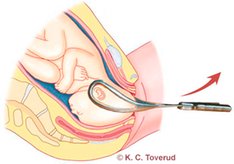
Expulsion phase
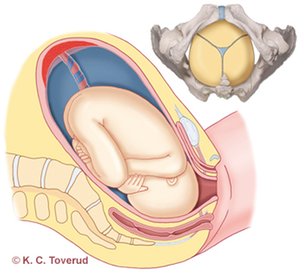
This is the phase of childbirth during which you actively push the child out. The child’s head has moved well down into the birthing canal and you feel the pressure down below. The cervix has now dilated 10cm, being fully open.
The need to push is a reflex that is triggered when the child’s head rests on the pelvic floor. As a rule, one will spontaneously begin to push. It comes naturally and automatically.
It is also usual for the midwife to guide and help one on how to do it. Most often, one fills one’s lungs with air and uses the air to create extra pressure when pushing the child out. You can try to push 2-3 times in this way with every contraction. It depends on the duration and strength of the contractions.
When you push, you will feel that the child’s head is moving further forward. It then slides back a little again during pauses between contractions. This can be a frustrating thing to experience, but it is very positive for the tissue, which can then stretch to make room for the child.
It is important that the child’s head be delivered carefully, so that the tissue has time to stretch, reducing the risk of tears. The midwife will guide you on how you can try to breathe instead of pushing right at the end when the child’s head comes out.
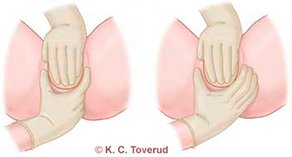
The midwife supports the genital tissue and guides the child’s head out.
Sometimes the whole child comes out with one contraction, but other times the contraction is over when the child’s head comes out. The midwife then dries the child and makes sure it is doing well. With the next contraction, the shoulders and the rest of the child come out.
After the child is born, it is dried well off, placed on its mother’s belly and covered with something dry and warm. The umbilical cord is cut when the blood inside it stops pulsating. The mother’s partner then receives the opportunity to cut the umbilical cord under guidance from the midwife.
Tears/episiotomy
In connection with childbirth, 85% of women experience injuries in the genital area. Most of these tears are superficial do no damage to the musculature.
If the child must come out quickly during the expulsion phase, an episiotomy is performed. In such cases, anaesthesia will first be administered.
Birthing positions
You can choose the position that you like best. Sometimes, a woman will be guided to into a certain position due to her progress in the birthing process or the child’s situation.
Giving birth in an upright position is positive in that one is then assisted by gravity and the contractions become more effective. In such cases, one often becomes more active and can better move one’s pelvis. One can give birth standing, using a birthing stool or squatting. Sitting in a squatting position or using a birthing stool is especially hard on the genital area. One can also stand on all four, which increases pelvic mobility.
In bed, one can lie on one’s side. This is good for flexibility of the pelvis and can, for example, work well when it comes to PGP (pelvic girdle pain).
One can also lie on one’s back/partially sit in bed. This a position that many make use of, feeling that it lets them use their energy in an effective manner.
It is normal to change positions while pushing, especially for women giving birth for the first time (nulliparous), as the pushing then often takes longer. Changing positions while pushing can in itself help cause the child to come out more easily.
It is important that you find a position where you feel that can make use of your energy in the best possible way. During this phase, it is important that you make a focused effort and push during the contractions, but also just as important that you relax well between the contractions and gather your strength.




Postnatal phase
This phase consists of the first hours after then child is born, when the mother is still in the delivery room.
The child is a new-born and quickly becomes cold. It is important that there be as much undisturbed skin-to-skin contact as possible and that the child is well covered. The child now needs calm surroundings and time to get to know the world around it.
Shortly after the child is born, the placenta will loosen. You may feel a contraction coming on and the placenta, as a rule, comes easily out if you press a little again. In rare cases, the placenta does not loosen on its own, but needs to be taken out under narcosis.
On the uterine wall, you will now have a soar the size of the placenta. To reduce the bleeding from it, it is important that the uterus contract well. This is something that the midwife takes care of. She will feel/squeeze your belly to make sure that it is happening.
After the child is born, the midwife examines the birthing canal to see if there are any tears that should be sewn up. This can be uncomfortable/painful after having birthed a child, but it is necessary in order to make sure that possible tears are not overlooked.
Reminder/to-do list for the birth
Remember to bring the following items with you:
- Your health card, blood-sample results, ultrasound form and any wish list
- Comfortable indoor clothing
- Indoor shoes
- Food for your companion during the birth
- A drinking bottle, if you wish to have one
- Toiletries
- A camera
- Music, reading material
- A cap for the baby and any other baby clothes
The midwife’s birthing aids
Wooden stethoscope
The stethoscope is used to hear the sound of the foetus’ heart. The midwife places the stethoscope on the pregnant woman’s belly and listens to the heartbeat.
The wooden stethoscope can be made of various materials, such as wood, plastic or metal.
TENS pain-relief device
Transcutaneous electrical nerve stimulation (TENS) is used to reduce pain.
Small electrodes are placed on your back, preferably on or near the area where there is pain. They send impulses through the nerves to the brain. You regulate their intensity yourself.
CTG-device
CTG (cardiotocography) is an electronic method of monitoring the child’s heartbeat and your contractions. The objective is to find out if the foetus lacks oxygen, so that if it does, birthing assistants can intervene before oxygen deficiency causes any damage.
Transducers are attached to the belly with bands, one which registers the sound of the child’s heart and one which registers tightening of the uterus.
The sound of the foetus’ heart is registered with the help of ultrasound signals. The contractions are registered with the help of an external pressure gauge. The child’s pulse can also be registered by fastening an electrode to its head after the water has broken.
On a display, one can read the graphed sound of the foetus’ heart and see how much time there is between contractions. Both are printed out on paper or shown on a screen.
The examination lasts from a half hour to an hour. Sometimes, CTG is used continuously in connection with childbirth.
STAN-device
STAN is a method of electronic monitoring which is used in addition to the well-known CTG (cardiotocogram) if a birth is risky at term to analyse the foetus’ ECG (electrocardiogram). ECG is gauges the functioning of the heart and is used, amongst other things, to see if there is any oxygen deficiency in the heart’s musculature.
If you are in the active phase of birth and monitoring of the foetus with STAN is indicated, an electrode will be placed on the foetus’ head after the water has broken.
An electrode will be fastened to your thigh. For registration to take place, you must have a belt over your belly. Everything will be connected to a STAN-device.
Support from a companion
As a rule, you will feel a need to receive support from the midwife and your companion during the active phase of childbirth. It can be a good idea to talk to your companion before the birth takes place about what kind of help you expect to receive from him/her while you are giving birth.
Loving care from your companion in the form of comforting or motivating words and physical touch (massage, stroking) can really help. It is important that you feel you are being taken care of by the midwife, that you are well-informed, that you get good advice and that you feel secure.
Your companion can also provide practical support, like helping you with food and drink, helping you find good resting positions or seeing to it that you make it to the restroom regularly to empty your bladder.
To you who are to be a companion during childbirth
Try to approach the situation as calmly as possible! Take responsibility for practical things like make sure there is enough fuel in the car, for example, or that you bring a telephone, a camera, a wallet, papers and the birthing bag with you when you go to the maternity ward, so that she does not have to think about such things. Remember to bring food for yourself, especially for during the night, when the kiosks are closed.
It is a good idea to prepare yourself for the childbirth taking time and being patient. Make sure that you take a few, short breaks, preferably outside of the birthing room, and get a breath of fresh air if you need to. It is important to communicate well with staff at the maternity ward. Do not be afraid to ask questions or communicate your wishes.
Through trial and error, find out what is helpful to the expectant mother and be prepared for possibly being rejected. Do not give up if you are, but keep trying. Maybe something else will work better.
In the following video, you will find many useful pointers on what approach you should take as a companion:
Pain relief and pain management
Pain is often a signal from the body that something is wrong. Birthing pains are an exception.
The following video provides more information on how you can manage and reduce pain during and after childbirth:
Childbirth is a complicated, but normal, bodily process. The pains are a result of pressing and stretching nerves, musculature and tendons. Many of the nerves affected in the process cause feelings of pain in the lower belly and back. As the birthing process proceeds, the pains will move down toward the genital area. As the expulsion phase approaches, the pains will often increase in intensity and somewhat larger area will be affected. The pains often change in nature during the expulsion phase, centralise in the lower region and radiate down through one’s legs.
Various things can contribute to affecting how you experience birthing pains. Knowledge about what is happening in one’s body helps to make one feel secure. Fear and anxiety increase one’s negative experience of pain. In preparing for childbirth, it is also important that you learn about different methods of pain relief and how they work. You can thereby gain a better overview and be in a better position to choose the methods which are right for you.
One’s companion in childbirth is often an important person when it comes to pain relief. The person with you is the person who knows you best. It should be a person who you feel secure in relation to and who gives you support and encouragement along the way. The person can communicate your thoughts and wishes in the course of the birthing process. He/she can also assist when it comes to massage, changing positions, movement and relaxation.
Pain Management
You yourself can influence your own experience of childbirth. It is important that you be well prepared, have knowledge about what is to happen and feel secure. In addition, it is important that you have support persons there with you during childbirth, ones who contribute in a positive way. A positive attitude toward childbirth has a positive effect on the process which you will go through. It is important that you believe in your own body and its ability to carry out a childbirth. Mobilise your strength and positive energy as the time approaches, doing so in something of the same way that an athlete prepares for a competition.
Breathing/relaxation
It is important to breathe calmly and evenly during childbirth. This cause one to be more relaxed. Breathe deeply and calmly deep into your belly. You can practice this at home before giving birth. Sit in a quiet place, make contact with and control your breathing through taking calm, deep breaths. Try to avoid thinking about anything else besides feeling how it causes your body to be calm.
Self-hypnosis
You can also employ self-hypnosis techniques – affirmation, where you find words or sentences which give you strength, help you to relax, stay calm or find motivation. Some examples include: ‘My body is made to give birth’ and ‘Together, we can do this – I, the baby and my partner’.
Visualisation
You create pictures within you which contextualise your experience of pain and give it meaning (for example, every contraction is a bucket of water which must be poured into the tub and when the tub is full, the baby will come). Imagine that you are in a quiet place where you feel secure.
Suggestion
Instruct yourself to achieve a desired bodily response. Focus inward, for example, so that the world around you becomes distant, or imagine that your body is heavy and relax well, so that the baby has a lot of room.
Movement
This is something that most do automatically. When we feel pain, we begin to walk around or rock. Most find that this reduces pain. This may be because the nerves are affected differently in upright position than while lying. Being upright and changing positions positively affects one’s progress in the birthing process, as well as the child’s movement down through the pelvis.
Massage
Many women find being massaged during childbirth to be agreeable and pain-relieving. You can be massaged during the entire birthing process wherever you feel it to be most effective. For example, having the bottom-most part of one’s lower back massaged often feels good. The intensity and strength which women prefer often varies. Skin sensitivity changes during childbirth, causing one’s experience of massage to change with it. Touch releases endorphins (the body’s own morphine), which increases circulation of the blood, makes the skin less irritable, reduces tension and relaxes one.
Water
Many find that water can have a good pain-relieving effect. You can use the shower or be in the bathtub. The water has a relaxing effect on one’s musculature, thereby causing one to experience the contractions as less painful. In the bathtub, many also find that their bodies feel lighter and that there is less pressure on muscles, joints and the genital area.
Rice bag
Having a warm covering over the area where it hurts most can also reduce pain well. It has something of the same effect as water, but to a lesser degree, as it affects a limited area.
Support and encouragement
It is important that those who are in the birthing room give support and encouragement to the woman giving birth. Childbirth is hard work that can be long-lasting and energy-intensive. Providing psychological support is an important task for both the woman’s companion and hospital staff.
Transcutaneous electrical nerve stimulation (TENS)
This is form of high-frequency electrical nerve stimulation that is not painful. Electrodes are fastened on one’s back and connected to a device. It can feel like a light vibration and you can control the intensity yourself. The method has no side effects.
Acupuncture
The needles are set by midwives with special competence and approved training in the area. Acupuncture can be used before, during and after childbirth. There are no risks or side effects. The effectivity is due to the sting of the needle releasing endorphins, as well as in part to it competing with the birthing pains.
Sterile water papules
Sterile water can be injected at several points over an area where pain is felt. This can have a pain-relieving effect for approximately 60-75 minutes. It can be a little painful when the needles are set, almost like the sting of a wasp, but aside from this there are no side effects.
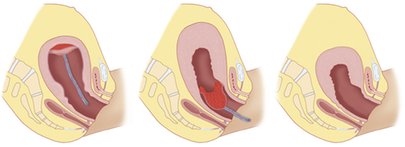
Epidural
This is a method of pain relief that is very effective. It is recommended in special cases, such as if the woman has preeclampsia or there will be a breech birth. It is also very favourable if the childbirth will take a long time. Most can have an epidural and the pregnant woman can have one if she wishes to.
An illustration of an epidural. The illustration is protected by copyright and cannot be downloaded. An epidural is applied to the back between two vertebrae by an anesthesiologist. A needle is inserted into the back and a thin, plastic hose is placed through it. When the hose is in place, the needle is pulled out, leaving only the hose behind. One then receives a painkiller through the hose until the childbirth is over. The medicine one receives numbs the roots of the nerves, so that one experiences relief from pain. This means that an epidural has the greatest pain-relieving effect during the cervical dilation phase, but not so much of an effect during the expulsion phase. This is advantageous in that you can feel when and how to push the child during the expulsion phase.
An epidural can have some side effects, such as a drop in blood pressure and pruritus (itch). Some can have problems urinating and approximately 1% experience spinal headaches. In addition, it can lead to the contraction stopping up a bit, causing the birth to take longer. If this happens, contractions will be stimulated to ensure that progress is made in the birthing process.
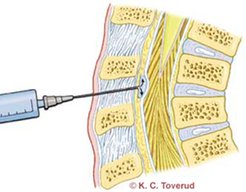
Use of obstetric forceps and ventouse (suction cup)/vacuum extraction (VE) is a little more frequently in childbirths where the women giving birth have received epidurals.
Post-term and labour induction
The due date is set through ultrasound imaging carried out around the 18th week of gestation by the NCFM (National Centre for Foetal Medicine) at St. Olav’s University Hospital’s Centre for Women and Children.
The due date is to be considered approximate.
We call a delivery ‘term’ if the baby is born between week 37 and week 42 of gestation. Most (approximately 70%) are born within the period lasting from a week before to a week after the term ultrasound (TUS) date. Very few women give birth on the term date itself. Moreover, approximately 25% are still pregnant a week later. A birth is post-term if it takes place more than 2 weeks after the expected term. At that time, 8-10% of women are still pregnant.
Labour Induction
At your last pregnancy check-up (in week 40 of gestation), you will receive information from the midwife regarding further check-ups and possible labour induction.
It is best for the mother and child if labour begins on its own. Nevertheless, there may in some cases be grounds for inducing labour. The most important indications for labour induction include, for example, that the child has grown too little, that it has too little amniotic fluid or that the woman is still pregnant more than 14 days after the TUS (term ultrasound date).
Labour can be induced in various ways. You will receive information at the hospital on the topic of labour induction if it is relevant in your particular case.
Procedures
Caesarean section (C-section)
Indications for a caesarean section include the following:
- The child’s condition (interpreted on the basis on foetal monitoring), slow progress, a previous caesarean section, breech position
Various divisions
- Planned (elective) caesarean section: the decision to carry out a caesarean section is made more than 8 hours before it is carried out
- By urgency (emergency caesarean section): the decision to carry out a caesarean section is made less than 8 hours before it is carried out
- By hyper-urgency (immediate emergency caesarean section): carried out as soon as possible, often under full narcosis
Planned caesarean sections are usually carried out 7-10 days before term. You must go to the pregnancy policlinic beforehand and speak with a midwife and doctor from the Childbirth and Anesthesia Department. In speaking with them, you will be given information on what happens before, during and after the procedure. You must bring a urine sample. Also, any necessary blood-samples will be taken the same day.
You can read more about caesarean sections at St. Olav’s University Hospital’s webpages.
Childbirth with the help of obstetric forceps or ventouse
In Norway (2006), 1.5% of all children were delivered using obstetric forceps and around 7.5% with ventouse (suction cup)/vacuum assisted vaginal delivery. In the western world in general, the percentage is 5-15%. Whether or not to use obstetric forceps or ventouse is a matter that can be considered at the maternity ward by the doctor or midwife as the birthing process proceeds.
Indications for the use of obstetric forceps
The child’s condition (assessed on the basis of monitoring of the child’s pulse), slow progress, long pushing time
It is the doctor who decides if there is a need to help the child out. It is also the doctor who assesses whether or not to use obstetric forceps or ventouse. You will receive information and guidance regarding the matter as you proceed if it is relevant in your particular case.
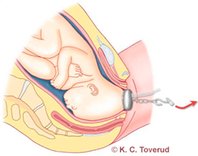
Breech position
At term, approximately 3% of all foetuses in Norway are positioned in the womb with their buttocks facing downward.
In week 36-37 of gestation, all pregnant women are to be examined to see what position the foetus is in. St. Olav’s University Hospital offers to attempt to turn the foetus around to head-first presentation in week 37. Any such an attempt will take place at the hospital, where doctors will try to rotate the foetus externally. Any need for further follow-up will be assessed on an individual basis.
In the birthing room after delivery
During childbirth, hospital staff endeavour to make the situation as calm as possible. This is done in an effort to avoid disturbing the mother while she is carrying out the work of childbirth. Calm is also important after the child is born, not only for child, but also for the new family as a whole.
By calm is meant the absence of unnecessary loud noises, dimmed lighting and no disturbing elements (mobile telephones, for example). You are now in a new situation. Try to live a little in the moment. You are both tired. It can be good to relax a little and gather oneself after giving birth.
The foundation for breastfeeding is now being laid as breastfeeding starts.
After you have relaxed and the child has been breastfed, the child will be weighed and measured. You will receive food. After you have eaten, it is important that you go to the restroom and try to urinate. Due to pressure on the bladder during childbirth, this can be difficult for some. If you wish to do so, you can take a shower. Of course, the decision to shower or not depends on how you are feeling.
Beginning to breastfeed
When the child is born, it is placed on its mother’s belly for skin-to-skin contact. This is a perfect point of departure for beginning to breastfeed. When the child can lie calmly there and calm surrounds it, it will eventually begin to seek its mother’s breast on its own.
One first notices that it begins to cluck out loud a little. It then sucks on its hands and begins to try to find its mother’s breast with its head. During this period, the child is very awake and attentive. It is important to take advantage of this and get breastfeeding started at this time.
One can help the child to one’s breast, so that it gets a firm sucking grip and can begin to suck. If you are uncertain about how to go about doing this, remember that you will get good help and guidance regarding it from staff at the hospital.
When the child is to suck on its mother’s breast, it is important that it have a good grip - this to say, one with as much of the brownish area around the nipple in its mouth as possible.
Please watch the breastfeeding videos at ammehjelpen.no
The child sucks powerfully and one can see the sucking movement all the way back to its ear. The first breast milk is yellowish in colour. It contains many antibodies that are important for the child. After breast feeding for the first time, the child often becomes sleepy and may sleep for a long time. When the child is awake, it is important that it be given the chance to suck on its mother’s breast. This causes the amount of breast milk produced to be adjusted in accordance with the child’s needs. When first starting out, it is normal to breastfeed every 1.5-3 hours during a 24-hour period. This is very hard on the breast and often leads to soreness. A proper sucking grip helps to prevents this. It can also be a good idea to smear a little breast milk around the nipple after breastfeeding and let it dry in the open air.
Some women report not having their babies placed on their bellies immediately after delivery (in cases where caesarean section have been performed, for example). In such cases, the child has been placed with its father, preferably in skin-to-skin contact with him. When the mother is ready for it, breastfeeding can be started as described above. When the child is awake, one undresses it, places it in skin-to-skin contact with its mother’s chest and lets it begin to search for a breast. When one sees that the child is interested and that it has begun to search, one can help it to find the breast and let it suck on it. During this period, time and calm are important. Getting a good start to breastfeeding helps to prevent breastfeeding problems later on.
The First Days after Childbirth
Start with pelvic floor exercises, preferably while lying in bed. It can be difficult to make contact with you pelvic floor musculature again after childbirth due to the swelling/stinging/pain/numbness. Start by pinching around your anus. Thereafter, see if you can get a hold of the muscles around your vaginal opening. It is normal for this to be difficult during the first days after childbirth, but there is no reason to wait to do so.
Continue to exercise your pelvic floor musculature, and start to exercise your abdominal muscles as well, preferably carefully. You can to this by flexing your deep abdominal muscles while lying down (bend your legs and put your feet on the mattress) and pushing your lower back against the mattress for a few seconds. Repeat the procedure a few times and gradually increase it with time.
Until about 6 weeks after childbirth (8-10 after a caesarean section)
It is still important that you get enough sleep and rest. It can be good to take a walk with your child in a pram. Continue the pelvic floor and abdominal musculature exercises described above. Wait with sit-ups/press-ups and tougher abdominal exercises.
From about 6 weeks after childbirth (8-10 after a caesarean section)
As a rule, the uterus has now returned to its normal size and the cleansing bleeding has generally stopped. Normally, the body is now ready for challenges that are a little bigger. When it comes to exercise, think simply. You don’t necessarily need to work out at a fitness centre!
Continue the pelvic floor exercises. Check to see that you have control over these muscles when upright and in motion as well before starting other exercise activities. Proceed carefully when it comes to running and jumping. Your pelvis may still be unstable or your pelvic floor musculature too weak, so that you may experience incontinence if you engage in such activities. Increase physical conditioning gradually by doing things like taking longer walks of greater intensity or going uphill.
Before beginning to do sit-ups/press-ups, your abdominal musculature should already have fallen together again in the middle of your abdomen. You can check to see if it has by flexing your abdominal muscles and feeling to see if there is still much room between them. If there is, you should wait to do sit-ups/press-ups.
You can begin doing general strength training exercises, preferably at home in your sitting room together with your child.
If you breastfeed and work out very intensely, so that you produce lactic acid, there will also be an increased level of lactic acid in your breastmilk. This can cause it to taste different, in turn causing some children to reject it. In most cases, it is sufficient that you milk out 2-5ml before taking your child to your breast. You can avoid having to do this by working out moderately.
Be careful not to wear an overly tight training bra if you breastfeed, as it can pinch your lactic ducts, as well as send your breasts signals that they are full and reduce milk production.
Breastfeeding and nutrition
The Norwegian Directorate of Health recommends that infants receive breastmilk as their sole sustenance during their first six months of life, at least insofar as it works out well for both the mother and the child grows as it should. After the first six months, the child should continue to receive breastmilk for the rest of its first year of life, or even longer, but together with additional food.
You can find information on breastfeeding in the pamphlet entitled How to Breastfeed Your Child, which is published by the Norwegian Directorate of Health:
helsedirektoratet.no
As regards proper nutrition for breastfeeding mothers, the Norwegian Food Safety Authority, in cooperation with the Norwegian Directorate of Health and other cooperating partners, provides information on the topic that can be found here:
Information on breastfeeding in other languages:
Breastfeeding Help [Ammehjelpen] is a politically neutral volunteer-based humanitarian organization that works to protect and promote breastfeeding. The Norwegian National Advisory Unit on Breastfeeding is a close cooperating partner of Breastfeeding Help.
Here is a link to breastfeeding videos from Breastfeeding Help: ammehjelpen.no
Here is a link to advice on medicinal use for pregnant or breastfeeding women: tryggmammamedisin
Breastmilk substitutes
Not all women can breastfeed, and some do not wish to do so. According to Guidelines on Postnatal Care in Norway, roughly ten percent of infants are bottle-fed a breastmilk substitute three months after birth. Some children receive pumped breastmilk. Some receive breastmilk, others a combination of breastmilk and a substitute for it.
How can I assess whether or not breastfeeding is going well? Here is a link to a breastfeeding check-list for mothers to use during the first weeks after childbirth:
Here is a link to the Maternity ward at St. Olav’s University Hospital:
The New-born Child
Congratulation on your baby! A new-born child needs much love and care. As a new parent, you are starting a new phase in life. Although you’ll become an expert on your child fairly quickly, it’s sometimes good to get some professional advice and guidance.
At the helsenorge.no website, you’ll find useful information on new-born children and how to follow them up after coming home:
- helsenorge.no/etter-fodsel
- helsenorge.no/spedbarn/omsorgen-for-det-nyfodte-barnet
- helsenorge.no/other-languages/english
Here is a link to information on jaundice in new-born infants: helsenorge.no/sykdom/blod-og-lymfe/gulsott-hos-nyfodte
Physical Activity after Childbirth
Physical activity can provide extra energy during the postnatal period, and it feels good for one’s body and soul. But keep in mind that you just went through both pregnancy and childbirth! Also, you now have a new-born child to spend your time on and get to know. During the first weeks after childbirth, you will need much sleep, rest and time to adjust to your new situation in life.
In beginning physical activity again, it is important to be careful and to do so only gradually. If you were not very physically active during your pregnancy, it is especially important to give your body time to get back in shape. Both your pelvic floor and your abdominal muscles are stretched after pregnancy and childbirth. Furthermore, your ligaments are affected by hormones, so that your joints will still be unstable.
The First Period of Time at Home after Childbirth
The first period of time after childbirth leads to a new situation in life and can present new challenges. Children need a day-to-day life characterized by care and predictability. This requires that the child’s caregivers have enough energy and that they are capable of caring for it. During the postpartum period, it is recommended that a woman rest much and that she maybe sleep when the child does. Her partner often has the opportunity to be at home during the first period of time after childbirth. He is an important support person for the woman and caregiver to child. If the woman is alone, it is desirable that she have the opportunity to receive support from another adult, be it a family member or a friend. If a woman has problems resting or sleeping after returning home, she can contact her local public health clinic or general practitioner for possible follow-up.
One’s feelings can swing much, both during pregnancy and the postpartum period. One is especially vulnerable during the postpartum period and it is important that one receives help and support that is customized in accordance with one’s needs. Every year, as many as 10-15% of all postpartum women in Norway experience a depressed mood or depression. Often, it manifests itself through anxiety or restlessness. Many of the women’s partners also struggle during this period. Some of the most common symptoms show up as a depressed mood, reduced concentration or ability to pay attention, distress or anger, sleep problems, exhaustion or pains, changed eating habits, lasting inner stress, sadness, a feeling of guilt, etc.
If you or your partner experience any of these symptoms, please contact your midwife, public health nurse or general practitioner. Support and help for you as parents can help to make day-to-day life better, both for you as parents and for your child. It can help give your child a good and secure start in life and improve the ties between it and you as its parents.
In accordance with national guidelines, one home visit by a midwife within the first or second day after returning home from the birthing institution is recommended. Furthermore, it is recommended that the number of home visits one receives be individually adjusted in accordance with one’s individual needs. As of the present time, Trondheim Municipal Authority has not implemented this particular recommendation.
One’s public health nurse will always offer to visit one at home in the course of the first 7-10 days after childbirth. A family’s local public health clinic will automatically contact it in the course of the days immediately after it is discharged from the birthing institution.
If you as parents need advice or guidance during weekends and/or in the evening time, please contact the emergency ward. During the first two weeks after childbirth, it is possible for you to contact St. Olav’s University Hospital.
stolav.no/no/Om-oss/Avdelinger/Fode/Barsel-vest/94455
During the first days or week after childbirth, bleeding from one’s uterus is natural. Such bleeding is, amongst things, referred to as cleansing. Tenderness and swelling in the genital area can also be due to tears or clipping (episiotomy). It heals quickly, often in the course of the first week after childbirth.
Care of the New-born Child
At the website helsenorge.no, you can find useful information on new-born children and how to follow up your new-born child after returning home:
helsenorge.no/spedbarn/omsorgen-for-det-nyfodte-barnet
helsenorge.no/other-languages/english
Information on jaundice in new-born children
Sexuality and Cohabitation during the Postpartum Period
Sexual feelings and needs change throughout life. Pregnancy, childbirth, the postpartum period and the young-child phase are a period of time that can present one with various challenges.
Childbirth effects sexuality and cohabitation in various ways. Roles change, not only those that partners play in relation to one another, but also those that they play in relation to their families, friends and acquaintances.
During the time after childbirth, the woman will have a need for rest and relief. Breastfeeding, bleeding, hormones and a new situation in life lead to her quickly tiring and lacking energy. Her partner is an important person when it comes to providing her with support and relief. It can be a good idea to limit visits from others and not plan too many activities during this period.
The woman and her partner may experience both physical and psycho-social changes after having become parents. Sexual desire can express itself differently after childbirth, in both women and men. One may also lack sexual desire for a variety of reasons, including:
- Discomfort due to tears or clipping (episiotomy)
- Bleeding from the vagina
- Dryness in the vagina due to hormonal changes as a result of breastfeeding
- Much loose, excess skin on one’s abdomen
- Incontinence
- Pain during sexual intercourse
- Pain during orgasm
- Fatigue
- Fear of waking the child
- A change in the hours one keeps
here are great individual differences when it comes to when one is physically and mentally ready to start having sex again after childbirth. There is no single answer, but it is recommended that one use a condom during the first six weeks after childbirth to avoid getting an infection. One should not have sexual intercourse if it feels wrong or becomes difficult, as doing so can negatively affect one’s sexuality. Sexuality encompasses much more than intercourse. Many desire closeness and intimacy without it necessarily involving penetration (penis in vagina). It is something that one will need to talk about and possibly explore.
Many studies have been done on when couples resume having sex after childbirth. Many of the studies done on postpartum women and their partners indicate that the interval of time between childbirth and when they start to have sex again varies widely from one couple to another. Most couples wait until 6-8 weeks after childbirth, but many wait much longer than this.
If you wish to avoid getting pregnant, it is important that you use birth control. A condom is perhaps the simplest method to use during the first weeks after childbirth, but there are many other types of birth control available as well. Contact your midwife or general practitioner to discuss which of the various types of birth control would be best suited to you and your partner. Here is some information on various methods of birth control:
sexogsamfunn.no/prevensjon/prevensjon
A woman and her partner may find that much of their need for care and closeness can be met through their child. This may in turn reduce the closeness and care for one another that the couple previously shared. It is important to prepare for this period by talking to one another about the expectations and thoughts that one has in relation to oneself and one’s partner. Openness is important if a couple is to be able to help one another during a time such as this, when one often has more questions than answers.
Please contact your local public health clinic, general practitioner or others that can help if you have a need to do so.
Sist oppdatert: 16.05.2025